Home › Forum Online Discussion › Practice › Human echolocation (video etc.)
- This topic has 5 replies, 1 voice, and was last updated 6 years, 5 months ago by
c_howdy.
-
AuthorPosts
-
March 1, 2019 at 3:01 pm #58340
c_howdy
Participant-https://allendaleacupuncture.com/2018/04/20/beating-the-heavenly-drum-qigong-exercise/-
I discovered this exercise only a few weeks ago after I did a frantic research on tinnitus for my patient. Turned out to be this “Beating the Heaven Drum” is an age-old Taoist Qigong exercise, practiced mostly by Taoist monks in northern China. This exercise is refuted to be a valuable tool in aiding and maintaining a healthy ear, hearing mechanism, and maintaining a clear mentality. There are two ways to do this exercise.
July 9, 2019 at 6:57 am #58853c_howdy
Participant
 July 19, 2019 at 2:15 am #58873
July 19, 2019 at 2:15 am #58873c_howdy
Participanthttps://www.youtube.com/watch?v=5S1wgzmGrTY
One should be thankful with what one has.
HOWDY
-https://en.wikipedia.org/wiki/Sometimes_I_Feel_Like_a_Motherless_Child-
“Sometimes I Feel Like a Motherless Child” (or simply “Motherless Child”) is a traditional Negro spiritual. It dates back to the era of slavery in the United States. An early performance of the song dates back to the 1870s by the Fisk Jubilee Singers. Like many traditional songs, it has many variations and has been recorded widely.
 July 31, 2019 at 2:24 am #58891
July 31, 2019 at 2:24 am #58891c_howdy
ParticipantImproved Prosthetic Hand Has A Lighter Touch And Easy Grip
July 24, 20192:59 PM ETKeven Walgamott, a real estate agent who lost his left hand and part of his arm in an electrical accident in 2002, got emotional when he was able to clasp his hands together and “feel” the space between his thumb and his index finger using a 3D-printed prosthetic hand in 2016.
“That was the first time I ever felt anything in my left hand since my amputation,” Walgamott says. He got emotional a second time when he was able to grasp his wife’s hand and “feel” her touch, this time through a newly designed, experimental prosthetic hand that can be directed with the user’s mind.
Walgamott was the sole volunteer for a 14-month study conducted by a multidisciplinary team based at the University of Utah, and also included collaborators from the University of Chicago and the Cleveland Clinic. The findings were published Wednesday in the journal Science Robotics.

The research team adapted a commercially developed prosthetic named the “LUKE arm” — after the robotic hand the character Luke Skywalker got in the Star Wars film The Empire Strikes Back.
The original LUKE arm had been designed to perform a variety of movements, but the Utah collaboration significantly improved it by figuring out how to mimic the way the human brain sends a signal to the hand to touch an object, and how the hand sends a signal back in response to touching it.
“The nerves that communicate and control the hand and the nerves that send information back up to the brain still exist even after the hand has been amputated,” explains Jacob George, a doctoral student of biomedical engineering at the University of Utah and one of the lead authors of the study.
The research team implanted electrodes in some of those nerves in Walgamott’s forearm and then recorded the signals that occurred when he thought of moving his hand to grab or touch an object. The prosthetic hand moved as commanded by Walgamott’s brain.
“The whole ‘using feedback for prosthetics’ idea has been floating around for a while and people just haven’t shown whether or not it works,” says Sharlene Flesher, postdoctoral research associate at Stanford University, who also studies tactile feedback in prosthetic robotic limbs, but was not involved in this study. “The fact that they got everything to work is not a trivial result.”
Other existing prosthetics can also convert brain signals into movement. But doing daily life tasks depends not only on our ability to grab objects but also on our ability to sense through touch what those objects are without looking at them.
For instance, if you try holding an egg in your hand while blindfolded, you’ll likely know right away that you have to handle it carefully to avoid breaking it. This is because the nerves in your hand send signals to your brain that tell you — based on past experience and characteristics such as shape, texture and heft — that you’re holding an egg. But with most prosthetic hands you’d need visual clues to tell you how strongly you could grip the object to avoid dropping it or crushing it.
The University of Utah researchers and their colleagues were able to restore Walgamott’s ability to “feel” what he was touching by providing stimuli through electrodes implanted in his arm; the information was quickly transmitted back up to the brain as if it were coming directly from the hand.
By recovering some of his sense of touch in this way, Walgamott was able to precisely distinguish between large and small and soft and hard objects after roughly 10 seconds of handling them — even when his eyes or ears were covered.
“We’re tapping into the same [mechanism] that’s used in my body and your body and everyone’s body, and we’re trying to just activate it in the way it would have normally been activated. So the sensations feel like they’re coming from their hand,” says George.
Walgamott says the sensations he experienced with the robotic hand didn’t feel exactly the same as those from his other hand, but he still found the ability to touch, feel and manipulate fragile objects like grapes and eggs astounding.
“Being able to pick up an egg without crushing it was a remarkable experience,” he says, and the skill translated to challenges he faces in daily life. Using the prosthetic in the lab, he was able to feed himself and load a pillow into a pillow case, and put on his wedding ring.
“This study kind of pushes the importance of why we should have sensorized prosthetics,” says Flesher. Beyond all the remaining technical challenges, she says, getting insurance companies to recognize the importance of such devices will be a key hurdle to overcome.
Insurance companies “think of it as a luxury,” Flesher says. “But [a sense of touch] really is so critical to how you control your arm.”
Prosthetic hands that can restore one’s sense of touch are currently not available outside the lab — Walgamott participated in the study for 14 months, wearing the prosthetic device for only a few hours per session during that time, and only in the lab. It connected to his arm via surgically implanted wires that were removed when the 14-month-long study was completed.
Using the device required a researcher’s direct supervision. For the LUKE Arm to be routinely usable at home, researchers would like to come up with a device that can be implanted inside the body, like a pacemaker. Though Utah companies are working on a wireless version of the device, it has only been tested in animals so far.
George and his collaborators hope next to get approval from the Food and Drug Administration to begin testing their modified LUKE arm in larger groups of people, and in the participants’ own homes instead of the lab. They are now testing a prosthetic arm whose electronic controls can be strapped to the waist, which would make it easier for patients to use without supervision.
Walgamott’s burning phantom pain — a pain coming from the hand that is no longer there – also was reduced while his prosthetic hand was turned on.
“[We are] recreating that sense of touch that they would normally be getting,” George explains. “When we start to do that, we think that we’re recreating the sense associated with that hand, [which] can kind of get rid of the pain.”
Unfortunately, Walgamott says that the pain was reduced for only about an hour after taking the prosthetic off, and then the pain returned with the same intensity as before. He continues to feel that pain today.
“Getting rid of phantom pain is one of the hopes,” a member of the research team told Walgamott during the experimental trial, according to a study transcript. “It’s not a promise. But if we restore sensory and motor function, then the prosthetic hand will become your hand, and the phantom will not have a place anymore.”
Luisa Torres is a AAAS Mass Media Fellow on NPR’s science desk.
 October 2, 2019 at 2:15 pm #59420
October 2, 2019 at 2:15 pm #59420c_howdy
ParticipantOCTOBER 2, 2019
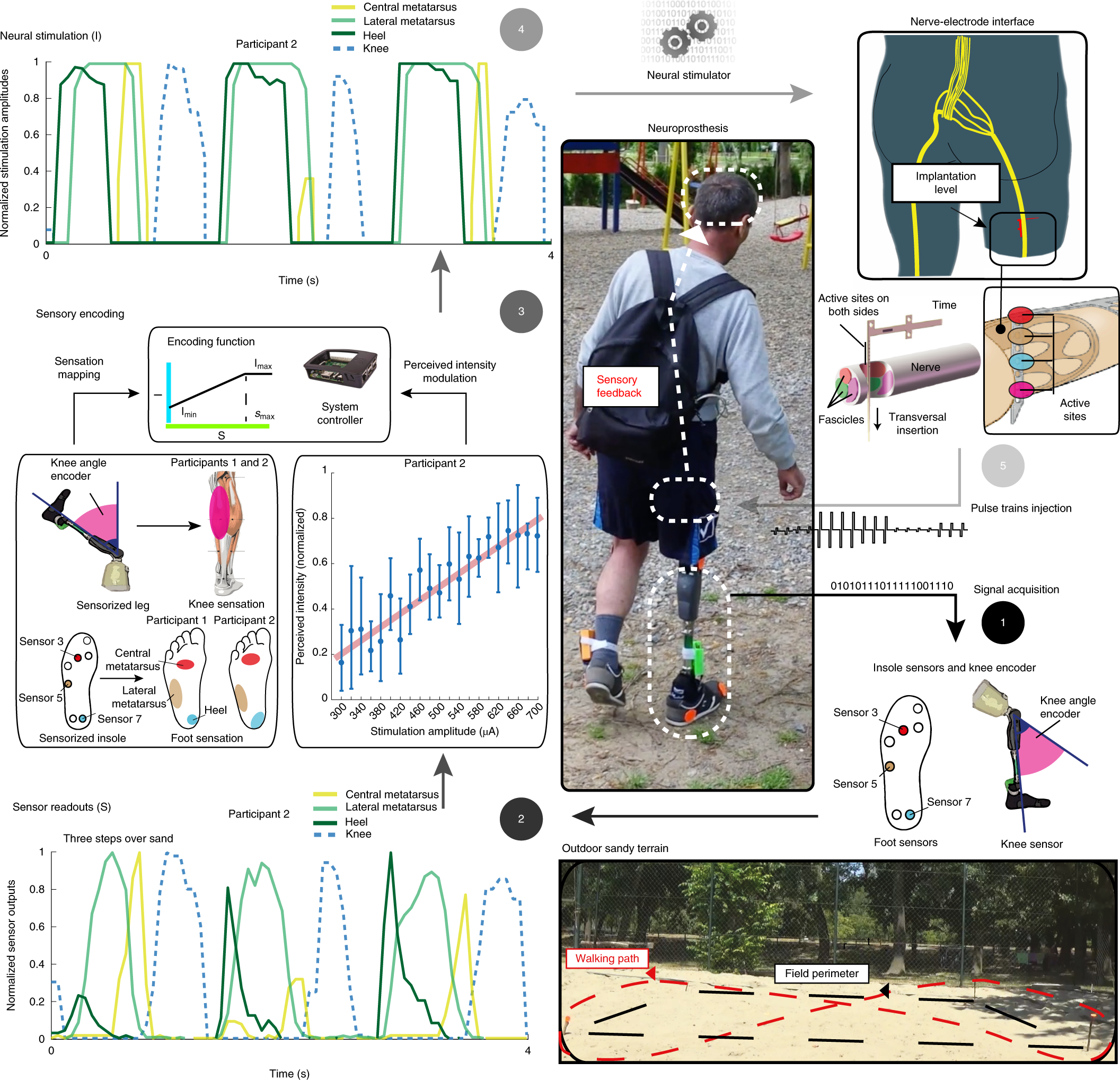
Leg amputees feel and use nerve-stimulating leg prosthesis as a real limb
by ETH Zurichhttps://medicalxpress.com/news/2019-10-leg-amputees-nerve-stimulating-prosthesis-real.html
A European consortium led by ETH Zurich and SensArs Neuroprosthetics reports that tiny electrodes implanted in a patients’ thigh nerve allow them to feel natural sensations of touch and movement from a prosthesis. Amputees can then walk freely while thinking about activities other than controlling the device. The details of the work were published in Science Translational Medicine and represent a multidisciplinary collaboration among several European institutions.
Djurica Resanovic, one of the volunteers, says, “The first time that I felt my leg, my foot, it was very interesting, like my own leg, after several years.” Wearing a blindfold and earplugs, Resanovic could tell where the foot was being touched, or how much the knee was flexed. “I recognized when they touched thumb, heel or foot, anywhere else.”
A sensorized insole is placed under the prosthetic foot. The signals from the insole and prosthetic knee sensors are translated in impulses of current, the language of the human nervous system, which are delivered to the residual peripheral nerve through tiny electrodes implanted transversally into the nerve itself. Then, the signals from the residual nerves are conveyed to the brain, which is able to perceive what happens at the prosthesis and to adjust the walking accordingly. The machine and the body are connected. Regaining limb awareness allows the subjects to feel obstacles underfoot and to avoid falls.
“We developed the first leg with feelings for highly disabled, above-knee amputees, which enabled them to surpass unexpected obstacles without falling, or to climb stairs much faster. These two tasks are extremely difficult, if even possible, for amputees wearing commercial prostheses,” said Stanisa Raspopovic, professor at ETH Zurich.
Leg amputees, while walking, do not trust the prosthesis and rely too much on the healthy leg, reducing mobility. The prosthesis, not being connected with the brain, doesn’t feel as a part of their body.
Brain activity measurements and psychophysical tests revealed that the neuroprosthesis is perceived as an extension of the body, as a real limb. The connection between the machine and nerve is fundamental to achieve this.
“You don’t need to concentrate to walk, you can look forward and step, you don’t need to look where your leg will fall.” says Djurica Resanovic, volunteer in the study. “The bionic leg integrated with the residual nerve of amputees enables the brain to accept it as the continuation of the natural leg, and this is essential for higher confidence of the users, and a future widespread of such technology,” Raspopovic said.
“An investigation longer than three months, with more subjects, and with in-home assessments should be executed to provide more robust data to draw clinically significant conclusions about an improvement of the health and quality of life of patients,” says Francesco Petrini.
More information: F.M. Petrini el al., “Enhancing functional abilities and cognitive integration of the lower limb prosthesis,” Science Translational Medicine (2019). stm.sciencemag.org/lookup/doi/ … scitranslmed.aaw3163
Journal information: Science Translational Medicine
 October 5, 2019 at 6:41 am #59429
October 5, 2019 at 6:41 am #59429c_howdy
ParticipantHow I broke a wine glass with my VOICE (6:55(57)…)

-
AuthorPosts
- You must be logged in to reply to this topic.
